The 2024 EU Digital Decade report reaffirmed what many HSE beneficiaries already suspected: The state of Ireland’s e-health systems is woefully underdeveloped. Launched in February 2025, the HSE Health App marks a significant milestone in the digitalisation of Ireland’s health. The App’s initial functionality is limited, but it does take steps to improve doctor-patient communication. However, the App’s failure to design for inclusivity could threaten to undermine efforts towards health equality in Ireland.
In many ways, Ireland is a European digital leader: 72.9% of the Irish population has at least a basic level of digital skills, massively outpacing the EU average of 55.6%. Multinationals have leveraged Ireland's highly educated workforce, advantageous corporate tax rates, and position as the EU’s sole English-speaking country to set up European headquarters throughout the country.
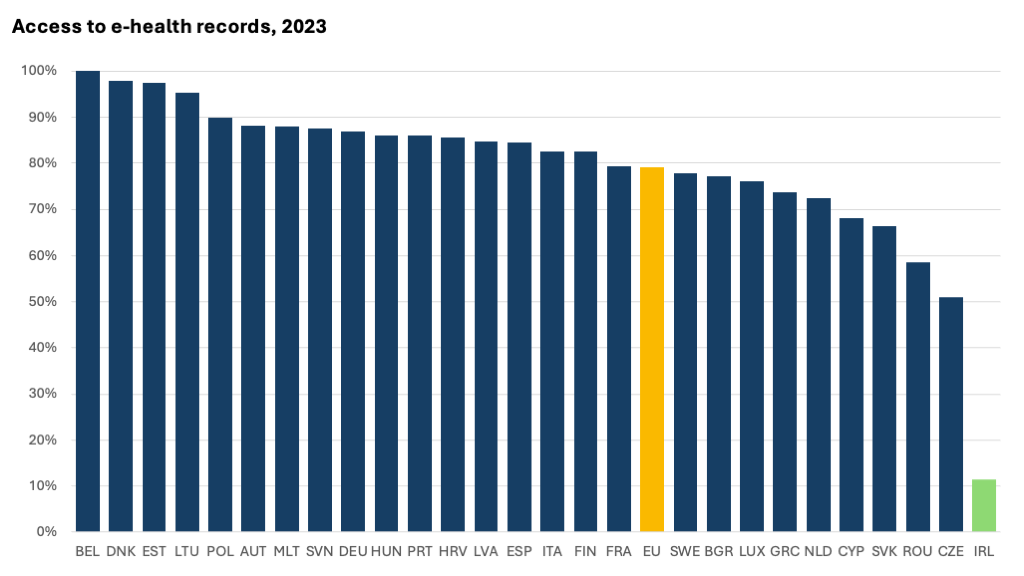
However, Ireland’s underdeveloped e-health system is holding the nation back from achieving a stronger digital future. The EU Digital Decade sets a goal of achieving universal EU citizen access to their electronic health records by 2030. According to the most recent EU eHealth survey examining 2023, Ireland was only 11.4% on the way to reaching this goal – far below the EU average of 79%. This score ranks Ireland last when compared to all other EU countries. These limitations challenge Ireland’s ability to share electronic health records internationally per EU recommendations.
Launching HSE Health App
Ireland remains the only EU member state without an online portal for accessing electronic health data—but that may soon change. The newly launched Health Service Executive (HSE) Health App, introduced on February 25 by the HSE and the Department of Health, represents a significant first step toward closing this gap.
As one of the initial milestones of Digital for Care 2030, Ireland’s health and social care digital framework, the app was developed with support from a range of private-sector contractors and service providers.
The App is available for free to anyone over age 16 with a MyGovID account. First-phase functionalities are most expansive for pregnant people and allow users to:
- Carry a list of self-declared medications and see a list of medicines received through the Drugs Payment Scheme or Medical Card Scheme.
- Store European Health Insurance Card, medical card, long-term illness card, Drug Payment Scheme Card, and GP visit card.
- Access flu and COVID-19 vaccination records.
- Find information on HSE services.
- View maternity service appointments.
Releases slated for later in 2025 will expand functionality for non-maternity patients, including access public hospital and screening appointment details, check referrals and waiting times, and receive self-care support for smoking cessation and chronic disease management.
Steps Towards Digital Maturity: Benefits of the HSE App
MyGovID Integration
The HSE Health App incorporated MyGovID, a centralised online platform commonly used for accessing government services and managing personal information. This integration leverages broad familiarity with MyGovID to enhance user accessibility and consolidating existing App technology allows for the secure storage of basic health information in one place.
Communication Facilitation
The App could facilitate improved communication between users and medical staff. Accurately recalling and verbally communicating medication history can be challenging, especially for patients who take several medications, experience communication barriers, or have memory difficulties. Assuming the App is reliable, in-App records could address these barriers, especially during high-stakes situations such as emergencies.
Promising Functionality Expansion
The App’s future functionalities are promising, including real-time wait times for Emergency Departments and Injury Units, as well as referral and waiting list details for non-maternity services. This could streamline healthcare by reducing the need for patients to contact doctors for updates and enabling those with hospital options to choose the shortest wait time
While the timeline for product expansion remains unclear, the App is expected to eventually allow individuals to designate a family member, carer, or trusted person to help manage their healthcare once the National Shared Care Record is fully implemented.
Key Challenge Areas
Challenges to Inclusion
Certain groups are more likely to experience challenges with this platform due to factors such as digital literacy, access to compatible devices, and a lack of universal design. Low-income households may lack smartphones or compatible devices, while shared-device users are limited by the App’s one-profile-per-phone setup. Rural populations may struggle with connectivity, and older adults and people with disabilities may encounter usability barriers, such as the need for screen readers, voice control, or alternative navigation. Language accessibility is also limited, as the platform is only available in English and Irish, excluding those who speak other languages.
In its App Accessibility Statement, the HSE acknowledges and commits to resolving the App’s accessibility shortcomings by April 2025. This transparency around the App’s accessibility is important and, hopefully, demonstrates a commitment to enhancing the usability of the App for all.
However, some barriers to access are built into the App by design and thus unlikely to be resolved. Access requires a verified MyGovID account, which in turn requires a Personal Public Service (PPS) number and Public Services Card—excluding new arrivals, young adults, and others without these credentials. Until these barriers are addressed, the App remains inaccessible to some of those who may need it most.
Legal Transparency
The Health Identifiers Act 2014 provides the legal framework for the introduction and management of individual health identifiers (IHIs) in Ireland. Within Ireland’s digital public services framework there is no transparent pathway showing how the IHI and MyGovID are working together. Not discussing the use of IHI and MyGovID together is a problem because it creates gaps in Ireland’s digital public services strategy, particularly in healthcare access and identity management.
Record Continuity
Record continuity within the App remains questionable. The App is only available for patients over age 16, but it is unclear whether childhood health records are included within the system once a patient becomes eligible. Parents and guardians therefore are not supported in accessing their dependents’ records. This could have a significant impact on patients with chronic health conditions who may need ongoing care or follow-up and access to their childhood records to inform care in adulthood.
Additionally, some "children’s" services, like CAMHS, are available to those over 16, with plans to extend access to under-25s. Key questions remain: If a referral to CAMHS or similar services is made before 16, will it appear in the App at 16? Will users have access to referral details and wait times?
Acknowledging private health providers
The App does not account for Ireland’s high reliance on private healthcare, with 47.6% of the population holding private insurance in 2022. It also excludes public patients referred to private providers to ease wait times, such as those using the HSE’s GP Access to Community Diagnostics (GPACD) Scheme. Despite over 700,000 scans being completed under GPACD in 2024, these records remain inaccessible via the App. It is unclear whether future integration with private providers will allow for a unified health record system.
Larger connection to health equity
The HSE Health App represents an important step toward modernising Ireland’s healthcare system, but its impact must be measured not only by technological advancement but also by its contribution to health equity. Access to digital healthcare services can reduce barriers to care, improve efficiency, and empower patients to take an active role in managing their health. However, if these tools are not designed with inclusivity at their core, they risk deepening existing inequalities rather than alleviating them.
To ensure that digital transformation in healthcare serves all communities equitably, future development of the App by the Government and contractors must include a strong commitment to accessibility. This means:
- Addressing the Digital Divide: The government must work to expand device access and digital literacy programs, particularly for older adults, low-income individuals, and people with disabilities.
- Ensuring Universal Design: Features such as screen reader compatibility, voice navigation, and multiple language options should be prioritised.
- Expanding Data Integration: The App must eventually integrate records from both public and private healthcare providers to reflect Ireland’s mixed healthcare model.
- Evaluating Impact: Regular assessments should track usage patterns, patient experiences, and disparities in access to ensure that the App is benefiting all demographics.
The rollout of the National Shared Care Record could play a transformative role in bridging these gaps. If implemented effectively, it has the potential to unify patient records across GPs, hospitals, and private healthcare providers, ensuring that no group is left behind in the digitalisation of healthcare. Additionally, Ireland must align its e-health strategies with the European Health Data Space to guarantee interoperability across EU healthcare systems, further enhancing patient rights and data accessibility.
Dr. Adeelia Goffe Adeelia Goffe

Current Research
Adeelia Goffe is the senior researcher for health. Her work centres on topics related to health and social care access pathways and associated outcomes for marginalised groups. She is currently working on social prescribing in vulnerable/marginalised communities and migrant health needs.
Research Themes
- Health inequalities
- Social determinants of health
- Social inclusion
- Marginalised/vulnerable groups
- Infectious disease epidemiology
Background
Adeelia has a PhD in Biology from the Georg August University of Göttingen (Germany). She also has degrees from Roehampton University (UK) and Cornell University (USA). She has published and refereed in international journals in behavioural ecology and virology. Prior to joining the TASC team, she worked on a number of research projects for the HSE and has lectured at Trinity College.
Molly Newell

Molly Newell leads TASC’s research on a variety of emerging tech issues, including AI, cybersecurity, digital regulation, and platform economies. An experienced project manager, Molly has led research teams analysing technology, cybersecurity, and security policy. She holds an MSc in Digital Policy from University College Dublin and a BA in Public Policy & Leadership from the University of Virginia.
Maria (Marysia) Pachowicz

Maria (Marysia) Pachowicz is TASC's Junior Researcher on Health. They have a B.A. in Psychology & Mathematics and an M.Sc. in Applied Psychology from Trinity College Dublin. They have conducted research on body image and disordered eating among sexual minority women for their undergraduate thesis, and on the experiences of accessing mental healthcare among people diagnosed with borderline personality disorder for their Masters thesis. They are a member of the “Sharing the Vision: A Mental Health Policy for Everyone” Reference Group of Service Users and Family Members, where they advise the Department of Health on the implementation of mental health policy, ensuring that the voice of the service user is at the centre of all decisions. They also sit on the Health Research Board Expert Group tasked with producing Ireland’s first National Mental Health Research Strategy. Aside from this, they have experience of working in disability services, as well as extensive experience in activism, particularly in relation to LGBTQ+ rights in Ireland and abroad.
Share:

![Duggan, Vic]](/assets/img/2017/04/1491994913319631_sq.jpg)
